Depression
Depression, or unipolar depression, is a problem characterized by an extremely sad mood that lasts for a long period of time and a lack of interest or pleasure in doing things that usually makes a person happy.
Someone with depression also has problems sleeping (either sleeping too much or too little); trouble thinking and concentrating; low levels of energy; unexpected changes in weight (either gaining or losing weight); and feelings of nervousness or agitation. With severe depression, there can also be recurrent thoughts about dying or actual suicide attempts.
If people experience these symptoms for at least two weeks, they might be diagnosed as having a major depressive episode. When left untreated, some major depressive episodes last as long as nine months, on average. After a depressive episode ends, the person might return to feeling normal. However, after experiencing the first major depressive episode, the odds of experiencing a second one increase by 50 percent, and with each new episode the odds only get worse that depressive episodes will keep coming. This is why getting treatment for depression is so important, even if the person’s most recent depressive episode has ended.
It’s important to remember that depression is not a sign of weakness or an inability to cope with normal problems. Most people with depression can’t effectively treat the problem by themselves; they have a very pessimistic view about themselves, the world, and life in general. People with depression think of themselves as incapable of handling their problems, which is both a result of the disorder and perhaps part of its cause. Regardless, depression is a very serious problem that can affect anyone.
When people are suffering with depression, there are probably many days when they don’t feel like getting out of bed. Either they feel too tired or maybe they think, “Why bother?” since life in general feels hopeless or pointless. Throughout the day, people with depression feel sad, blue, sluggish, unmotivated, and empty inside, like there’s a part of themselves that’s missing. They might even experience headaches or body aches for which there are no apparent causes, feel restless and agitated, and find it difficult to concentrate.
In most cases of depression, the person no longer has an interest in pleasurable activities, like hobbies, exercising, socializing, or even sex. Instead, the person might be preoccupied with thoughts about death and dying. It’s common for people with depression to think about ways to kill themselves. Some of them might even try to commit suicide. Others who are no longer concerned if they live or die might frequently take dangerous risks, like driving too fast or walking in traffic.
Depression can also cause many problems in people’s relationships, especially marriages and partnerships. Often, people who are depressed have problematic beliefs about their relationships. They may believe that they shouldn’t disagree with their partner, which puts added stress on both people. Others who are depressed seek constant reassurance from their friends and loved ones, which strains those relationships. People with depression will do this to determine if they’re doing the “right” thing or to find out if they’re still loved.
Unfortunately, no amount of reassurance from the nondepressed partner or friend ever seems to be enough. And in some cases, the constant reassurance seeking can lead to the nondepressed partner or friend also becoming depressed.
Another type of depression is dysthymia, a type of depression that’s longer-lasting and seems to stay with the person for his or her entire life. In some ways, dysthymia might not be as severe or disabling as a major depressive episode, because often the person can still function in everyday life. People with dysthymia also might not have as many problems with sleeping, thinking, or weight changes.
But because dysthymia is so constant and long lasting, it becomes a part of a person’s personality. A person with dysthymia might look generally unhappy or sad all of the time, and his or her mood might never return to a balanced, healthy state. A person with dysthymia might also experience depressive episodes at times, a condition known as double depression.
Officially, depression and dysthymia, along with the bipolar disorders, are collectively referred to as mood disorders.
Because untreated depression has the habit of repeating itself, and getting worse, one of the most serious consequences of the disorder is suicide. Between 20 and 35 percent of all suicides are due to depression. This doesn’t mean that every person with depression is going to attempt suicide, but it does mean that depression is a serious problem that needs to be treated.
Most people with depression or dysthymia also struggle with other problems. In reports such as the 2005 U.S. National Comorbidity Survey Replication, it’s been estimated that almost half of the people diagnosed with depression also struggle with mental health problems such as specific phobias, social phobia, generalized anxiety disorder, panic disorder, post-traumatic stress disorder, obsessive-compulsive disorder, dependent personality problems, and borderline personality disorder.
Many people with depression and dysthymia also battle drug and alcohol problems, which complicates treatment of both the depression and the substance abuse. A 2004 report in the Archives of General Psychiatry revealed that among more than forty-three thousand people surveyed in the United States, approximately 19 percent of those with depression also had a problem with drugs or alcohol, as did approximately 18 percent of the people with dysthymia.
In addition, many people with depression also have medical conditions, such as hypertension, arthritis, skin problems, cancer, speech disorders, heart disease, ulcers, and cardiovascular disease. Often it’s the development of one of these illnesses that leads to the onset of depression. However, there’s also evidence that the reverse can be true: If left untreated, depression can lead to problems like cardiovascular disease and heart disease, and if a person has already had a heart attack, depression can increase the risk of having another one.
A report published by the World Health Organization and the Harvard School of Public Health in 1996 stated that the worldwide impact of depression has long been underestimated and that it’s only getting worse. The report stated that by the year 2020, depression will be the number one cause of disability for women around the world. Plus, when both sexes are considered, depression will be the world’s second leading cause of disability, behind only heart disease.
In the United States alone, it’s been estimated that depression affects approximately 5 to 10 percent of the adult population every year, or approximately ten million to nineteen million adults. However, over the course of a person’s entire life the statistics get even higher. During the course of a lifetime, 5 to 12 percent of all men and 10 to 25 percent of all women will probably experience an episode of depression.
In general, women are usually diagnosed with the problem twice as often as men. Some researchers think that women are more vulnerable to depression due to factors such as hormonal changes during puberty, greater risk of experiencing anxiety, greater number of life stressors,33 and greater lack of social support.
Depression usually begins between the ages of fifteen and thirty for both men and women, but depression and dysthymia can also affect younger children. In the United States, the average age of onset for depression is twenty-seven for men and twenty-eight for women, with similar ages in other Western countries.
Dysthymia affects approximately 3 to 5 percent of the adult population at some point in their lives, or approximately eleven million Americans, and again, women are diagnosed with the problem about twice as often as men. Like depression, dysthymia can also begin at any point in a person’s life, but it usually begins between childhood and early adulthood.
The exact causes of depression and dysthymia are still unknown. However, there are many biological, environmental, and social risk factors that are known to influence the development of the disorder.
Heredity
Many people are born with a genetic risk for developing depression, which can then be triggered by social or environmental factors such as stress. Since the end of the twentieth century, scientists have been examining the genetic instructions that create the human body. One of the results has been the identification of similar genetic codes for depression in related family members. If a person has an immediate family member who is depressed, such as a parent or sibling, that person is one and a half to three times more likely to develop depression than someone without an immediate family member who is depressed. Similarly, dysthymia is more common in people who have a parent or a sibling who is depressed or dysthymic. But heredity is only a risk factor and not a definite cause; it only means that a person is more vulnerable to developing depression.
Biology
Brain chemicals called neurotransmitters also contribute to the development of depression. In particular, the neurotransmitters serotonin and norepinephrine appear to play key roles. Originally, it was thought that low levels of these chemicals in the brain caused depression, but more recent research suggests that it is more complicated than that. It’s now thought that these two chemicals might regulate other neurotransmitters, such as dopamine and acetylcholine, that might also contribute to depression.
Similarly, the hormone melatonin can play a role in depression. In winter, the decrease in sunlight causes the human body to produce more melatonin, which results in greater fatigue and the need to sleep more. Some people are affected more strongly by this surge of melatonin, resulting in a form of depression called seasonal affective disorder (SAD).
Illnesses
Illnesses can also cause depression, especially life-threatening and chronic illnesses. Very few people who are battling cancer, for example, are going to do so and not feel depressed at some point. Facing disease, and possibly death, is enough to make even the strongest person feel depressed. Additionally, certain illnesses create chemical changes in the body that cause depression or depression-like symptoms. These illnesses include multiple sclerosis, thyroid problems, cancer, influenza, hepatitis, tuberculosis, Parkinson’s disease, tumors, stroke, dementia, Alzheimer’s disease, and vitamin deficiencies. Women who suffer from premenstrual syndrome (PMS) or who have recently had a baby may also experience symptoms of depression. People who are suffering from depression and also experiencing one of these illnesses, or another illness that is suspected of causing depression, should consult a medical professional in addition to a mental health care professional.
Medications
Certain medications for other illnesses might also cause depression. These include the hepatitis medication interferon alfa (Roferon) and the arthritis medication indomethacin (Indocin). Additionally, some oral contraceptives can also cause depressive symptoms. People who are taking any of these medications and also experiencing depression should contact the health care professional who prescribed the medication. They should not stop taking the suspected medication without first talking to the medical professional. Stopping medication without medical advice might lead to more complicated and severe problems.
Other Substances
Many other substances can also cause depression. Alcohol, by its nature, is a depressant. At first, it might make a person feel relaxed, but if consumed in large enough quantities, it will make that person feel depressed. Many frequently used recreational drugs can also cause depression or depression-like symptoms. These drugs include marijuana, cocaine, heroin, diazepam (Valium), Ecstasy, and amphetamines. An excessive use of caffeine, which causes increased heart rate, anxiety, and irritability, can worsen a person’s depression. Many environmental toxins are also suspected of being linked to depression. These chemicals include pesticides, copper, aluminum, mercury, lead, and formaldehyde. People who suspect that they have been exposed to one of these chemicals, or to another toxic chemical, should consult a medical professional.
Trauma
Depression can also be caused by traumas in a person’s life. A trauma is any event that causes severe emotional or physical injury and leaves long-lasting damage. Some of the more common causes of trauma include war, crime, rape, accidents, abuse, natural disasters, and relationship problems.
It isn’t necessary for the trauma to have occurred recently for it to affect a person’s mental health. It’s possible for older traumas to cause depression, too. For example, children who experience any form of abuse are more likely to develop depression as adults, possibly due to the effects of stress on the nervous system at the time of the abuse. It’s also been observed that people who experience the childhood loss of a parent, to either death or divorce, are much more likely to develop depression as adults. (Interestingly, the early loss of a parent due to divorce, rather than death, appears to be a stronger predictor of depression.) Both of these types of experiences have very long-lasting impacts and might cause people to look at their lives and relationships in a very negative way, which eventually can lead to depression.
Finally, brain-imaging research has shown that, in general, traumatic events leave long-lasting impacts on the brain, especially on the parts of the brain associated with memory and emotions. These results seem to occur no matter when the trauma takes place in a person’s life. But because the brain is very fragile and still developing during childhood, any trauma that occurs during that time is bound to leave some impact on the person, no matter how inconsequential that trauma might appear later in adulthood.
Self-Defeating Thoughts
Depression can also be caused by repetitive self-defeating thoughts. The negative messages we replay in our heads are some of the most powerful obstacles we must overcome in our lives. Sadly, many of these self-defeating thoughts don’t even originate with us. Instead, they were told to us by our parents, friends, or society. Some of these thoughts might include “I’m not good enough,” “I’m unlovable,” or “I should take care of others instead of myself.” Anyone who hears messages like these often enough will usually begin to believe them, no matter how damaging they are. In other contexts, this process is called propaganda, brainwashing, and advertising, and we are all capable of being affected by it.
Interpersonal Conflicts
Depression may also be caused by feelings of not being connected with others or being in conflict with others. The feelings of being alone or unwanted are perhaps two of the most powerful emotions humans can experience. So it’s not strange that feeling them can lead to depression. These are very difficult feelings to deal with, especially when a person is alone or in an unsatisfying relationship. In fact, social isolation and lack of social support are two predictors of suicide in people with severe depression. People who think they have no one else to live for often don’t want to live for themselves.
Loss of Meaning
Depression can be caused by the loss of meaning in a person’s life. The meanings we give life can be religious, spiritual, community based, or personal. Sometimes these beliefs are challenged. Most of the time, people’s beliefs will remain strong or adjust to accommodate new information. However, sometimes meanings and beliefs fail, and as a result, people lose faith in their religion, country, society, or job. When this happens, it’s understandable that depression follows. If a person spends years investing time, energy, and commitment into something, that something becomes very powerful in his or her life. Then, if that something is suddenly shown to be wrong, or if the person begins to have doubts about what he or she was investing in for all those years, that realization may have a major negative impact on the person’s life. It might even cause the person to doubt himself or herself: “How could I have been so stupid? What was I thinking for all those years?”
Unresolved Grief
Lastly, it’s important to note that depression is not the same as mourning, although they may look similar. Many people will react in a way that resembles depression after someone they know dies. This is considered normal grieving. However, if the feelings of grief persist for an extended length of time or become worse, it might become depression. In this case, the person should consult a mental health care professional.
Regrettably, more than half of the people who need treatment for depression don’t seek help. For example, the 2005 National Comorbidity Survey Replication study of adults in the United States found that only 37 percent sought help for their depression within a year of the problem’s onset; and, on average, people waited eight years before seeking treatment for depression. This is unfortunate, considering that there are very effective treatments for depression that could help people avoid the long-term disability associated with the disorder. In general, more than 80 percent of the people who get appropriate treatment for their depression experience an improvement in their lives.
The majority of people who seek help for depression initially choose to take antidepressant medications. For some causes of depression, such as heredity, biology, illnesses, medications, and other substances, antidepressant medications might be the best initial treatment. In other cases, a combination of psychotherapy and antidepressants might be necessary, especially to treat chronic depression.
Among the more commonly prescribed antidepressants are a group of medications called selective serotonin reuptake inhibitors (SSRIs), which includes fluoxetine (Prozac), sertraline (Zoloft), fluvoxamine (Luvox), paroxetine (Paxil), and citalopram (Celexa). Other newer types of antidepressants include venlafaxine (Effexor), nefazodone (Serzone), mirtazapine (Remeron), and bupropion (Wellbutrin). In general, both these and other types of antidepressants need to be taken regularly for four to eight weeks before the therapeutic effects begin to take effect, and all of the medications have the potential of causing additional side effects.
Due to these complications, many people seek psychotherapy as an alternative or additional treatment. In many studies, certain types of psychotherapy have been shown to be just as effective as antidepressant medications, even for moderate and severe depression, And in some cases, psychotherapy succeeds where antidepressants fail.
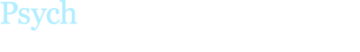
In multiple clinical studies, certain psychological treatments have been shown to be more effective than others at treating depression. These successful treatments include behavioral therapy, cognitive behavioral therapy, interpersonal therapy, and brief psychodynamic therapy. Smaller studies also suggest that acceptance and commitment therapy might be an effective treatment for depression.
Both behavioral therapy and cognitive behavioral therapy for depression focus on the ways a person’s actions can contribute to depression, while cognitive behavioral therapy also focuses on changing the person’s habitual negative thought patterns. For these reasons, these two types of therapy are often successful in treating depression caused by illnesses, other substances, trauma, self-defeating thoughts, interpersonal conflicts, and loss of meaning.
Cognitive behavioral therapy for depression has probably received the most research support of all the psychological treatments. It appears to be effective in approximately 45 to 60 percent of the cases studied, which is comparable to or better than the success rates of some antidepressants. However, when compared to the use of medications, cognitive behavioral therapy has been shown to be twice as effective at preventing relapse one year after treatment ends, due to people stopping the use of their antidepressants. Another advantage of CBT was found in a study reported in the Archives of General Psychiatry in 2004, which showed that cognitive behavioral therapy for depression leaves lasting improvements in the brain that are similar to the effects of taking antidepressant medication.
According to information published by the U.S. National Institute of Mental Health, both cognitive behavioral therapy and interpersonal therapy by themselves are effective for treating mild to moderate depression, while using either therapy in combination with an antidepressant seems to be the most effective treatment for severe depression.
Interpersonal therapy for depression focuses on how relationships and changing roles in life contribute to a person’s depression. For this reason, interpersonal therapy is often effective in treating depression caused by relationship conflicts, development of an illness, or mourning a lost loved one.
Brief psychodynamic therapy focuses on resolving internal struggles and relationship problems caused by interpersonal connections and conflicts. For these reasons, brief psychodynamic therapy is often effective in treating depression caused by trauma, interpersonal conflicts, and loss of meaning in a person’s life.
Acceptance and commitment therapy (ACT) is a relatively new form of psychotherapy that incorporates elements of behavior therapy and meditation and mindfulness practices. ACT is based on the principle that many psychological problems are caused by efforts to control, avoid, or get rid of emotions and thoughts that are undesirable. Consequently, the goal of treatment is to help people learn to accept experiences that cannot be changed, observe emotional thoughts without getting stuck to them, and commit to actions based upon what they value in life.
Couples therapy and family therapy have also been shown to be effective in treating depression caused by interpersonal conflicts, although they have not received as much clinical support as the other therapies.
And despite the lack of research support, many people have found relief using many other forms of psychotherapy, such as long-term psychodynamic therapy and humanistic therapy. These and other types of psychotherapies can often be helpful for treating depression caused by interpersonal conflicts and loss of meaning in a person’s life.
Other people have found relief using alternative treatments for depression. For depression caused by seasonal affective disorder, light therapy—exposure to sunlight or special sun lamps—is often effective. Physical exercise can also be effective. In 2002, the journal Psychosomatic Medicine85 reported a study of 156 adults over the age of fifty comparing the use of antidepressants with participation in an exercise regimen. Interestingly, the volunteers using each treatment improved and were no longer depressed at the end of the study. However, ten months after the study ended, volunteers in the exercise group had less of a chance of relapsing into depression, especially if they had continued to exercise on their own.
Additionally, some people have sought treatment for depression by using over-the-counter remedies such as Saint-John’s-wort. While there is some evidence that this can be effective in treating mild to moderate forms of depression, one large study sponsored by the U.S. National Institute of Mental Health found that the herb was no more effective than a placebo pill. In addition, Saint-John’s-wort has been known to interfere with the effectiveness of other medications, such as antidepressants and some oral birth control pills.
Lastly, perhaps the most drastic form of treatment for depression is electroconvulsive therapy (ECT), known more commonly as electroshock therapy. Usually, this is a last alternative for treating depression, used only when the disorder hasn’t responded to other forms of treatment. ECT is a hospital procedure in which a person is given a muscle relaxant and anesthesia before having an electric current sent through the body for half a second. This treatment is usually conducted six to twelve times and spread out over the course of two to four weeks. Many patients find relief from their depression using this treatment when other methods have failed, especially when their depression also includes delusional thinking.
Cognitive behavioral therapy (CBT) is a form of treatment that combines elements of both cognitive therapy and behavior therapy. Cognitive therapy examines the way people’s thoughts about themselves, others, and the world affect their mental health. Behavior therapy investigates the way people’s actions influence their own lives and their interactions with others. By combining the two, CBT examines the way people can change their thoughts and behaviors in order to improve their lives.
The CBT treatment for depression is generally composed of four steps:
- Conduct an assessment and provide education
- Get reactivated in life
- Challenge and correct self-defeating thoughts
- Prevent relapse
Step 1: Conduct an Assessment and Provide Education
The first step of the CBT treatment for depression is to conduct an assessment of the person’s symptoms in order to verify that he or she is struggling with depression and not some other similar problem. Once the person has been diagnosed with depression, it’s important that he or she understands the basic nature and causes of the disorder (as highlighted above). It’s also important to educate the person’s family and friends about the disorder in order to help them understand how they might be playing a role in maintaining the disorder, as well as how they might be able to help during the treatment. It’s also important for everyone involved to understand that CBT is an active form of treatment that requires the person with depression and his or her loved ones to do work outside of the therapy session.
Step 2: Get Reactivated in Life
The second step of the CBT treatment for depression is to help people begin scheduling pleasurable activities back into their lives. When people become depressed, they often isolate themselves from the rest of the world and avoid fun and interesting activities, which, ironically, only serves to deepen their depression. One of the most important initial steps of treatment, therefore, is to get people reactivated in life and help them stop avoiding activities. This can be done in many ways, but using a schedule to plan and record activities is often helpful and motivating.
Step 3: Challenge and Correct Self-Defeating Thoughts
The third step of the CBT treatment for depression is to challenge and correct self-defeating thoughts. These thoughts are often the cause of sad and hopeless feelings. At the most observable level are automatic thoughts. These are critical thoughts that people think and say to themselves that sabotage success and happiness. Two examples of automatic thoughts might be “I don’t deserve anything good happening to me” and “Why bother trying? I’m just going to fail.” A person can be either aware or completely unaware of having a thought like this. However, in both cases the result is that the person feels sad or hopeless.
Much of the CBT treatment for depression will be spent identifying and reevaluating these types of thoughts. This can be done with the use of a thought record. The thought record helps the person with depression look for evidence that both supports and contradicts these thoughts. Then, most importantly, it helps the person create a more balanced thought. For example, if the person struggling with depression had the thought “Why bother trying? I’m just going to fail,” the thought record would offer evidence of this thought being true and examples of it not being true in the person’s life.
The thought record also helps the person identify different types of cognitive distortions, unhelpful thinking styles that generate those automatic thoughts. For example, overgeneralizing involves making broad negative conclusions about life based on limited situations, and minimizing and magnifying involve discounting the positive and enlarging the negative aspects of life.
By evaluating the evidence and cognitive distortions, the goal of the thought record is to help the person with depression find a new, more balanced thought and ease feelings of sadness and hopelessness. In this example, perhaps a more balanced thought would be “Even though I don’t do everything perfectly, I’m still capable of doing most things pretty well.” And instead of feeling excessively sad, such as 8 on a scale of 1 to 10, perhaps this newer thought will help the person feel less sad, say only a 5 out of 10.
As the work on challenging automatic thoughts continues, a person using a thought record will usually begin to notice common themes among his or her thoughts. These themes often point to deeper, more firmly entrenched core beliefs about one’s self that make a person more vulnerable to depression. These core beliefs, often called schemas, include thoughts like “I’m a failure,” “I’m worthless,” and “I’m unlovable.” When these core beliefs are encountered, they too need to be challenged and modified using the thought record and other techniques.
Step 4: Prevent Relapse
Finally, the fourth step of the CBT treatment for depression is preventing relapse after treatment is complete. The key to relapse prevention is for the person to continue using the cognitive and behavioral skills learned in treatment and to recognize the early signs of returning depression in order to take steps to prevent relapse. And when needed, people should always consider seeking additional help from medical and mental health care professionals.
Interpersonal therapy (IPT) was developed in the 1980s as a short-term, structured treatment for depression. In some cases, IPT treatment may last for only twelve to sixteen sessions. However, longer treatment is often necessary.
IPT will help a person explore how depression is affecting his or her relationships, as well as how those relationships are contributing to his or her mental health problems. Relationships with romantic partners, family members, friends, and coworkers are all equally important in IPT and need to be examined. It might also be necessary to explore what was happening in the person’s life when the depression developed. But because of the time-limited nature of IPT, little emphasis is placed on exploring a person’s past beyond how it might be currently affecting his or her relationships.
The interpersonal therapy treatment for depression includes four steps; however, not all the steps are easily adaptable to self-help models of treatment. The second, third, and fourth steps might require the help of a mental health care professional. The five steps of the interpersonal treatment for depression are as follows:
- Conduct an assessment and provide education
- Make an interpersonal inventory
- Take on the “sick role”
- Define the focus of treatment
- Work through the problems
Step 1: Conduct an Assessment and Provide Education
The first step is to conduct an initial assessment of the person’s symptoms in order to verify that he or she is struggling with depression and not some other similar problem. Once people have been diagnosed with depression, it’s also important that they understand the basic nature and causes of the disorder (as highlighted above).
Step 2: Make an Interpersonal Inventory
The second step is to help the person make an interpersonal inventory. The interpersonal inventory is a diagram or a list of all the important people in the life of the person struggling with depression. This includes people from both the past and the present. Creating an interpersonal inventory is an important first step in identifying both the number and the quality of a person’s relationships. This will help later in mending strained relationships and building better social support.
Step 3: Take on the “Sick Role”
The third step is for the person with depression to take on the “sick role.” This means that the person acknowledges that he or she is dealing with a real illness, just like diabetes or cancer. The goal is to help people with depression stop blaming themselves for being sick and for not living up to their own or other people’s expectations. Defining the sick role in this way will hopefully free them up from other responsibilities and allow them to focus on taking care of themselves.
Step 4: Define the Focus of Treatment
The fourth step is to define the focus of treatment, whether it’s grief, interpersonal disputes, role transitions, or interpersonal deficits. When working in a time-limited treatment, it’s acknowledged that not all of a person’s problems can be addressed. It’s therefore beneficial for the person to focus on one specific area of his or her life in treatment.
Step 5: Work Through the Problems
Finally, the fifth and last step is to work through the problems in the defined focus of treatment. This begins by helping people link their feelings of depression to some interpersonal event that they have experienced. IPT generally focuses on four causes of depression: role disputes, grief, life transitions, and skills deficits.
When a person’s depression is caused by disputes and disagreements with others, the goals of treatment include learning how to negotiate and communicate in more effective ways. When depression is caused by grief for a loved one who has passed away, treatment includes the exploration of feelings for that person and reengaging with other people.
Changing roles in life can also cause depression, as it sometimes does during divorce, the development of an illness, or changing jobs. If this is the case, IPT can help the person explore his or her feelings about loss of the old role and identify new skills that are needed in the new role. And, finally, sometimes people experience depression because they don’t have skills to cope with issues like loneliness and isolation. In these cases, IPT can help people expand their social support network and learn other needed skills, such as assertive communication skills to handle interpersonal situations.
Acceptance and commitment therapy (ACT) incorporates elements of behavior therapy, meditation and mindfulness practices, and scientific research on how humans think and learn.
ACT (pronounced “act”) is based on the principle that many psychological problems are caused by efforts to control, avoid, or get rid of emotions and thoughts that are undesirable. Often, people try to get rid of feelings and thoughts that make them sad or anxious, just as they get rid of other things they don’t want, such as old clothes. However, as ACT points out, feelings and thoughts can’t be controlled. A person can’t throw them out like an unwanted pair of shoes. In fact, the harder a person tries to control his or her thoughts and feelings, the more powerful they often become and the longer they stick around.
The ACT treatment for depression generally includes eight steps:
- Educate about depression and ACT
- Develop self-as-context
- Utilize cognitive defusion
- Develop acceptance
- Focus on Contact with the Present Moment
- Clarify Values
- Commit to Taking Action
- Stay Committed to Values and Actions
Step 1: Educate About Depression and ACT
The initial step of the ACT treatment for depression is education. It’s important to educate the person and the person’s family members about the nature of depression and emotions like sadness. It’s especially important for the person with depression to understand these things from an ACT point of view. According to this treatment, it’s the person’s attempts to avoid and control certain emotions and thoughts that make depression an overwhelming problem. Starting with the early stages of treatment, it’s also important for everyone involved to understand that ACT is an active, participatory treatment designed to help the person live a more fulfilling life, not necessarily a “happier” one.
Step 2: Develop Self-As-Context
In ACT, to develop “self-as-context” means to participate in the events of life but also feel independent of those events and their outcomes. People who have accomplished this feel secure in their ability to function in the world. They don’t become entangled in the thoughts and emotions of daily events. When people are able to participate in experiences and simultaneously separate themselves from those experiences, they also become aware of opportunities to make healthier choices in life. Developing self-as-context often includes the use of metaphors and experiential exercises.
Step 3: Utilize Cognitive Defusion
Cognitive defusion is a mindfulness technique that helps people observe their sad and depressing thoughts without becoming attached to them. “Defuse” is an invented word that means to unstick or to unfuse one’s self from the words that arise in thoughts. The goal of this stage of treatment is to allow people with depression to function more freely without judging themselves, their feelings, or their thoughts. Thoughts and emotions often arise haphazardly, so it’s easy to see that depression could worsen over time if a person were to follow or believe every thought and emotion that arose.
Cognitive defusion is often accomplished using meditation or mindfulness techniques, such as imagining thoughts floating by on a cloud, repeating the words of a thought over and over until they lose meaning, or imagining a thought as something outside of oneself. By observing the process of thinking and feeling, the goal is to create space between the person and his or her experience. This gives the person more control over decisions made based on those thoughts and feelings.
Step 4: Develop Acceptance
In ACT, learning to accept frustrating situations and distressing emotions, like sadness, is the alternative to trying to control or avoid them. Acceptance can be hard, but it’s often the only way people can reclaim control of their lives. Many situations cannot be altered, no matter how much a person wishes them to be changed. Accepting this fact is often the first step in reengaging with life. Accepting what cannot be changed frees a person from struggling against it and allows that person to start taking actions based on what he or she values in life.
In order to cultivate acceptance, people are encouraged to experience the distressing emotions that they have been avoiding, to cease fighting things that cannot be altered, and to engage in situations that have been evaded.
Step 5: Focus on Contact with the Present Moment
Focusing on what’s happening in the present moment can help people develop more flexible coping strategies for handling fear and anxiety. When people dwell on the past, they often become sad, and when they anticipate the future, they often become anxious. In both cases, they miss what’s happening at the present time. Paying attention to what’s happening in the moment gives people more control over the decisions they’re making and allows them to see more possibilities in life. This skill is often developed with present-focused mindfulness skills, such as focusing on the rising and falling of the breath or on physical sensations in the body.
Step 6: Clarify Values
ACT acknowledges that life is often lived on autopilot, without much sense of what a person really cares about. Clarifying and establishing what a person values can often help that person live a more fulfilling life, despite occasionally feeling blue or sad. Values are the elements of life that give it meaning and importance, like “maintaining a loving relationship with my spouse or partner” or “being an active member of my community.” These values are like compass headings that guide a person through life. They are not destinations at which a person can ever arrive. A person can never stop maintaining a loving relationship and still have a loving relationship. Values are concepts that point a person in the direction of a fulfilling life, and ACT uses many types of values clarification tools to help people identify their values.
Step 7: Commit to Taking Action
After a person has determined his or her values, it’s important to establish goals that support those values and then commit to taking actions that fulfill those goals. For example, if a person’s value is to be an active member of her community, she might list a number of different goals to fulfill that value, such as “attend community meetings twice a month.” This is something that can be completed and thereby create a sense of valued living. The ACT treatment for depression includes development of skills and goals that lead to taking committed action.
Step 8: Stay Committed to Values and Actions
Finally, in order to create a fulfilling life, it’s crucial for people to continue making decisions based on what they value in life, rather than based on the thoughts and feelings they have tried to avoid in the past.
Disclaimer
This website is for informational purposes only and does not provide an official diagnosis. Anyone struggling with a physical or mental health problem should seek the services of a medical or psychological professional as soon as possible. Furthermore, if you’re having thoughts about suicide or hurting someone else, please see our crisis resources list, contact your local emergency services, or go to a local hospital immediately.
RECOMMENDED READING
The Upward Spiral
Using Neuroscience to Reverse the Course of Depression...