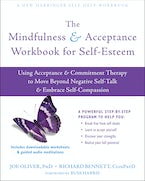
By Joe Oliver, PhD, and Richard Bennett, ClinPsyD
Lots of people say that we should be careful with what we do with the information we receive on a daily basis. ‘Don’t believe everything you read’ is a common mantra. We would add to that, ‘Don’t believe everything you think.’ Simply accepting the content of our thoughts as being true is pretty much the default setting for most of us, as relying on our minds is the result of thousands of years of human evolution. The process is not intrinsically problematic, since taking our thoughts literally and trusting in what they say is helpful to problem-solving and other practical uses of language in the world around us.
However, thinking something does not make that thing true or helpful, and believing everything our minds tell us can lead to problems, particularly when the content of those thoughts is excessively self-critical. Most of us, therapists and clients alike, have a version of the ‘not good enough’ story knocking around in our heads. And most of us have tried to reason or rationalize these thoughts away. But sometimes they are held on to so tightly that reasoning or rationalizing is just not possible. So, what can we do when this shows up in therapy?
Here are our top tips to help clients respond effectively to these thoughts:
Encourage clients to build greater awareness of automatic statements that suggest an equivalence between their sense of self and the thoughts they are having. For example, “I am not good enough” suggests that “I” and “not good enough” are the same thing. It’s like “I = not good enough.” It can be helpful to instead promote distinction between the two with the idea that your client is more like the thinker, rather than the thought. The following simple language convention can help build this distinction:
a. “I’m not good enough.”
b. “I’m having the thought that I’m not good enough.”
c. “I’m noticing that I’m having the thought that I’m not good enough.”
With each iteration, you may notice a distancing and reduction of the impact of the initial thought. Adding extra language in front of the unhelpful thought helps to promote a distinction between “I” and “not good enough.”
Catching up on the series? Read part two here.
Joe Oliver, PhD, is a consultant clinical psychologist and joint director of the cognitive behavioral therapy (CBT) for psychosis postgraduate diploma program at University College London. He also works within a North London National Health Service Trust, developing training and delivering interventions for people with psychosis. He is founder of Contextual Consulting, a London-based consultancy offering acceptance and commitment therapy (ACT)-focused training, supervision, and psychological therapy. Joe is an Association for Contextual Behavioral Science (ACBS) peer-reviewed ACT trainer, and regularly delivers ACT teaching and training in the UK and internationally. He is coeditor of Acceptance and Commitment Therapy and Mindfulness for Psychosis, and coauthor of ACTivate Your Life and Acceptance and Commitment Therapy.
Richard Bennett, ClinPsyD, works as a clinical psychologist and cognitive behavioral psychotherapist. He lectures at the Centre for Applied Psychology at the University of Birmingham, where he leads the postgraduate diploma program in CBT. He worked in adult and forensic mental health services in the National Health Service for over twenty years before setting up Think Psychology, an independent psychology practice offering therapy, supervision, and training. Richard is an active member of ACBS and the British Association of Behavioural and Cognitive Psychotherapies (BABCP). He is recognized as a BABCP-accredited psychotherapist, supervisor, and trainer; and an ACBS peer-reviewed ACT trainer. He coedited Rational Emotive Behavior Therapy in Sport and Exercise, and is coauthor of Acceptance and Commitment Therapy.


 2024 Peace Playbook: 3 Tactics to Avoid Clashes with Your Partner
2024 Peace Playbook: 3 Tactics to Avoid Clashes with Your Partner